Content Information
According to the ACS-COT (2014), it is the role of the TPM to, “monitor clinical processes and outcomes and system issues related to the quality of care provided; develop quality filters, audits, and case reviews; identify trends and sentinel events; and help outline remedial actions while maintaining confidentiality” (p. 43).
This may very well be the most important job function of the TPM. The continual monitoring, identification, and reconciliation of issues identified by the program that lead to suboptimal care of the injured patient is paramount in the development of a high-quality trauma program. When beginning to embark on a program for Performance Improvement and Patient Safety (PIPS), please reference Chapter 16 of the American College of Surgeons Committee on Trauma Resources for the Optimal Care of the Injured Patient 2014. This chapter provides operational concepts, program configuration, principals of PIPS, core measures, tables, and the criteria for a high-functioning trauma program. According to the ACS-COT (2014) “performance improvement activities are concordant with the Institute of Medicine’s six quality aims for patient care: safe, effective, patient centered, timely, efficient, and equitable” (p. 114). Other resource materials for high-quality PIPS include:
- Individual Hospital Quality Programs
- Healthcare Coalition Partners or Health Network Affiliates
- Institute for Healthcare Improvement – www.ihi.org
- National Academy of Medicine - https://nam.edu/
- American College of Surgeons Committee on Trauma - https://www.facs.org/quality-programs/trauma
- Society of Trauma Nurses TOPIC - http://www.traumanurses.org/education/stn-topic
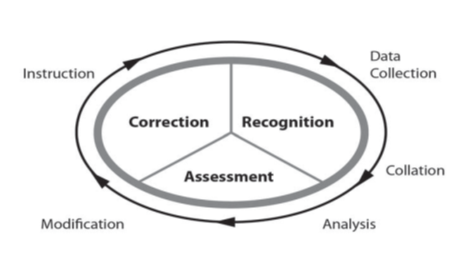
Figure 1 represents the continuous process of performance improvement. The ACS-COT (2014), “calls for each trauma program to demonstrate a continuous process of monitoring, assessment, and management directed at improving care” (p. 114).
There are always opportunities for improvement in all levels of trauma centers. High-quality health care is a constantly moving target and the less that is done to monitor, assess, and improve a trauma program, the farther the trauma program will be left behind. A football analogy is a great way to think about performance improvement (PI) and how it does not always originate from negative outcomes. Dr. Donald Jenkin’s football analogy reads: it is late in the fourth quarter and your team is down by 5 points. Your quarterback goes back to throw a pass. He is almost sacked several times, but manages to get the pass off. Meanwhile the receiver forgets his route, but manages to catch the ball on his fingertips while balancing on his toes on the side line. TOUCHDOWN and your team wins the game, so outcome good. But the play certainly didn’t go as schemed: the offensive line allowed pressure on the quarterback, the receiver ran the wrong route, and the pass was barely caught. The same concepts apply to trauma PI, there are many PI initiatives that can be worked on even when the outcome is good.
The general principle of Performance Improvement and Patient Safety (PIPS) is to improve the value of care delivered to the injured patient. This concept can be demonstrated with a simple equation:
Value of Care = Quality of Process + Quality of Outcome
Cost
According to the ACS-COT (2014):
- The value of care can be increased by improving the quality of process, improving the quality of outcome, or decreasing cost…the trauma program’s scope of performance evaluation extends from institution-wide variables (process review) to measures of individual practitioner performance (peer review). The determinants of how well a trauma center performs include variables that can be influenced (such as efficacy, safety, or cost of care) and variables that cannot be influenced (such as the severity of injury or preexisting co-morbidities) (p. 117).
As the TPM, it will be imperative that the formation of a comprehensive PIPS program is of the highest priority. A PIPS written plan must be in place for a trauma center to be verified at any level. A PIPS written plan establishes the structure of the PIPS program and how it is operationalized, ensures continuity and expectations for all participants in the process, is an educational tool for new staff, and outlines the linkage to the hospital-wide PIPS program. It should contain the following: the philosophy/mission/vision of the institution, the authority and scope of the program, the indicators/audit filters, a process for event identification, the management of data, the committee structure and membership, roles and responsibilities, the levels of review, peer determinations, corrective action planning and implementation, event resolution strategies and re-evaluation, confidentiality of data, and integration into the hospital-wide PIPS process.
The Iowa Department of Health and Human Services Trauma Coordinator presented a webinar titled, “Level III PIPS Presentation.” That presentation contains a thorough description of what should be contained in a PIPS written plan and how often it should be updated. The presentation also highlights the requirements for PIPS at a Level III facility and what is required for trauma re-verification as a Level III facility. Also contained on this website page are sample tools for use in a PIPS program.
The first steps in writing a PIPS plan are establishing authority for the program, establishing the team members and their roles and responsibilities, and formalizing links to the institutional PIPS program. Authority and scope for the PIPS program may look something like this:
Authority
- Administrative Leader - Active Voice in the C-Suite
- Trauma Medical Director
- Trauma Program Manager - Facilitator
- Hospital PI - open lines of communication
Scope
- TMD/TPM Authority to manage process
- TMD/TPM Authority for defining action plans/prevention
- TMD/TPM Authority for defining loop closure/event resolution
- TMD Authority for medical staff peer review
- Encompass all phases of care provided to the trauma patient
- resuscitation, diagnostic evaluation, admission, hospital course, rehabilitation, outcome or discharge
The committee structure and member roles and responsibilities may look something like this:
- Chair
- Co-chair
- Members:
- Surgery
- ER Liaison
- ICU Liaison
- Anesthesia Liaison
- Orthopedic Liaison
- Neurology/Neurosurgeon Liaison
- Radiology
- Laboratory
- EMS
The establishment of links to institutional PIPS may look something like this:

The trauma performance improvement patient safety (PIPS) committee is responsible for the trauma re-verifications and compliances for the facility. It is responsible for trauma patient clinical outcomes, processes of care, and coordination of care. It is responsible for formulating the PIPS plan and putting the plan into action. The PIPS committee is responsible for setting goals and reviewing the PIPS plan annually to ensure the plan reflects the most up-to-date standards and outcome measures.
After the committee membership, scope, authority and connections to the institutional PIPS are established in the PIPS plan, the process for adverse event identification can now be outlined. This section of the PIPS plan will answer the question, how does the TPM get notified of a trauma patient having entered into the hospital’s care at any point in time and how is an adverse event identified? Many TPMs work with their hospital’s coding/billing department and IT to establish reports generated through the electronic medical record in order to identify all trauma patients who meet inclusion criteria for the state trauma registry. After trauma patient identification, charts are then taken through the review process. A good way to establish consistent, non-emotional review of charts is through utilization of a chart audit tool. The chart audit tool will have benchmarks, set by the trauma program, for determining if the patient received expert care in a timely manner. This chart audit tool can help the TPM determine if an adverse event occurred or if the care of the injured patient did not satisfy the trauma program’s established benchmarks. The process for how the trauma program identifies patients, performs a consistent chart review, and can identify adverse events should be outlined in the PIPS plan.
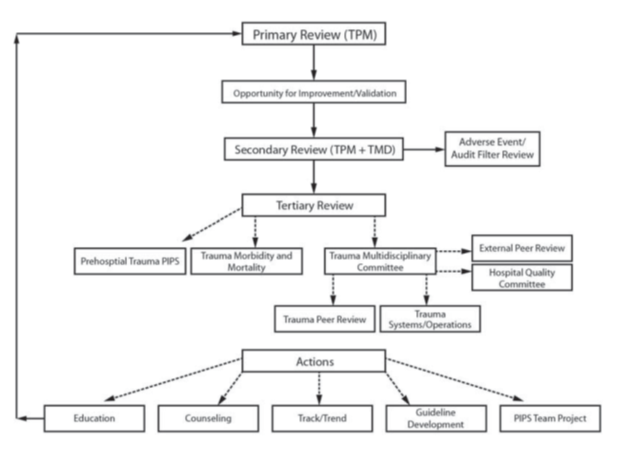
Figure 2. Trauma PIPS Levels of Review. This figure visually demonstrates the levels of review and the circular nature of monitoring actions for effectiveness of event mitigation (ACS-COT, 2014, p. 129).
After completion of the chart review, the PIPS plan should then provide direction on what level of review the chart should proceed. The levels of review for evaluation of charts is set by the trauma program. In general, the primary review is done by the TPM. This is that initial walk-through of the chart with the chart audit tool. If there are no issues identified that caused harm to the patient or all program benchmarks were met, review of the medical record may be complete at this time. No action or loop closure is necessary. If an event is found that did cause harm to the patient or if a program’s benchmarks were not met, then a secondary level of review should be performed. This secondary review is typically done by the TMD. After review by the TMD, an action plan or loop closure may proceed at this time. If the TMD determines the case should go to tertiary review for a provider issue, then the chart review is passed to the multidisciplinary peer review committee. If the TMD determines there is a system issue that needs to be brought for tertiary review, then the system issue is brought to the Trauma PIPS committee or passed to the director of the department in which the system issue was identified. This tertiary review can also be put through an external peer review process or even passed to pre-hospital EMS PIPS programs, depending on where the event occurred and who was involved. The responses from these tertiary reviews should be collected and continuously monitored for follow-up planning and assurance of loop closure. All of these steps should be outlined in the Trauma PIPS Plan.
The actions that can result from performance improvement reviews fall into any of several categories. Education, counseling, track/trend, guideline development, and/or a PIPS team project can result out of an effective PIPS process. These actions should then be monitored for their effectiveness of event mitigation.
An important factor in determining whether an event needs to pass to the secondary review or tertiary review is the level of harm. A level of harm can be determined to be no harm or no detectable harm, minimal harm, moderate harm, severe harm, or death.
- No harm is defined as the standard of care was provided with some deviations with no impact to the patient.
- No detectable harm is the event occurred but did not reach or impact the patient and no treatment was necessary.
- Minimal harm is defined as an impact to the patient, the patient is symptomatic, symptoms are mild, loss of function is minimal or intermediate by short term, and no or minimal intervention (extra observation, investigation review, minor treatment) is required.
- Moderate harm is when the patient is symptomatic, requiring an intervention and there is an increase in length of stay or long term loss of function, there may be a necessitation of higher level of care, but this can be expected to resolve prior to discharge.
- Severe harm is when the patient is symptomatic, requires a life-saving intervention or major surgical/medical critical care intervention, there may be a shortening of life expectancy or major permanent or long term harm or loss of function, there may have been an error in judgement, deviation from practice, or system delays which result in an impact to quality of care and quality of life.
- Death, of course, is when death was caused or brought forward by the event.
There should be a pre-determined level of review, set by the trauma program, which occurs at every determined level of harm. Primary, or level one reviews, typically would occur for all patients who qualify as no harm or no detectable harm. A secondary, or level two review, would then proceed for all subsequent levels of harm. And a tertiary, or level three review, would typically proceed for charts identified as those with an opportunity for improvement, where harm was determined to impact the patient, and that contain a provider issue. As the TPM works through this process the next step, after establishing what the levels of review are going to be for each established level of harm, is to develop or use a PIPS audit form that works for the level of trauma care facility. Contact the State of Iowa Trauma Coordinator for access to resources for chart audit templates, if there is not a template identified in the available online resources that would be appropriate for the trauma care facility. A PIPS audit form creates a standardized approach to chart review, it produces a non-emotional validation of the patient chart, it can be used concurrently or retrospectively, and it helps to determine the taxonomy of the event.
Determining event taxonomy helps the TPM lay out, in plain language, the impact to the patient, the type of event, the domain, the cause, prevention of the event, and determination of the event outcome. A great way to utilize the state trauma registry is to use the Performance Improvement tab for documenting the taxonomy of the event. The impact can be determined by the TPM. The impact denotes if the patient had any level of physical harm, psychological harm, legal issue, or socioeconomic (unnecessary treatment/procedure) impact. For example, if communication of the patient condition was inaccurate or incomplete, this field can be marked. The domain of the event, is where the event occurred. For example, pre-hospital, operating room or intensive care unit. The cause of the event, is the factors and/or agents that led to the incident as either system based or human based. And then prevention of the event has prescribed prevention efforts that can be chosen. The determination of the event can be system related or provider related.
Using the state’s trauma registry performance improvement tab can move the performance improvement of the facility to being fully electronic if utilized to its full extent.
The PIPS plan should also include how the facility is going to handle data management and confidentiality. Using words like “not discoverable” and “not public” or “confidential for peer review only” when using patient sensitive information during meetings and/or collecting meeting materials after meeting where confidential patient information is shared are some examples of safe patient information handling. Storing items in a secure location and use of generic identifiers, when able, is another way to protect patient sensitive information. These data management processes should be detailed in the PIPS plan.
After an event goes through the PIPS process there may be a corrective action plan created. This corrective action plan can either be system based or individual based or both. It is important to frame this corrective action plan as a SMART goal. A SMART goal is specific, measureable, achievable, relevant, and time-bound. This helps provide clear guidance and measurability to the corrective action and makes it easier to determine the effectiveness of the plan for future event mitigation.
The PIPS process is very involved, but is perhaps the most important role of the TPM. When programs are consistently adapted to overcome system or provider barriers it helps assure the optimal care of injured patients is consistent across the continuum of care.